Adaptation of AI in Cardiovascular Imaging: A Glimpse into the Future
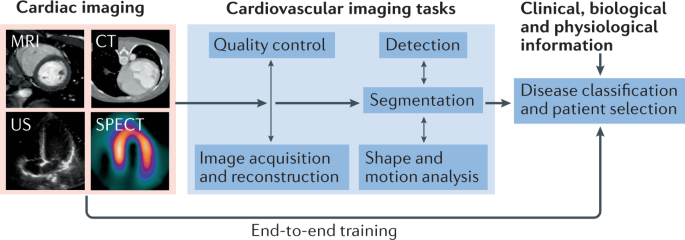
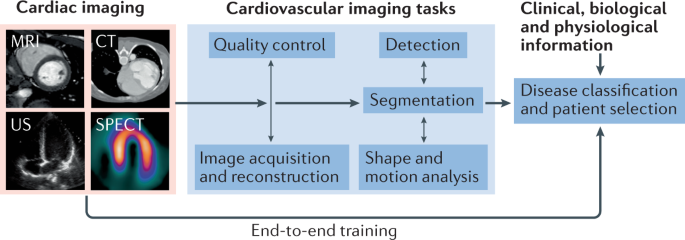
The integration of artificial intelligence (AI) with cardiovascular imaging marks a significant turning point in modern medical practice. Over the past several years, the blending of tools such as optical coherence tomography (OCT) with AI platforms has transformed traditional imaging techniques, offering physicians the ability to receive real-time, actionable insights. This evolving relationship not only enhances the precision of interventions, but also sets the stage for a new era of personalized, data-driven cardiovascular care.
Historically, conventional imaging methods like traditional angiography have been the cornerstone of cardiac diagnostics. However, these technologies often suffer from restrictions—namely, limited visibility deep within arterial walls and insufficient detail in plaque composition. In contrast, OCT provides three-dimensional images of vascular structures, giving doctors a more detailed roadmap for planning intricate interventions. When combined with AI, these images become more than just pictures: they are now the basis for fully informed decision-making, enabling the rapid assessment of vessel conditions and more precise selection of devices.
This opinion editorial will take a closer look at how AI-powered imaging is redefining cardiovascular interventions, review the challenges and opportunities along the way, and offer a perspective on preparing both healthcare facilities and professionals for this transformative technology.
Real-Time Plaque Characterization: Improving Decision-Making in the Cath Lab
One of the major benefits of integrating AI with OCT imaging is the ability to perform real-time plaque characterization. Traditional imaging techniques often leave physicians confronting tricky parts such as ambiguous plaque boundaries and unclear classification of tissue types. AI steps in to simplify these tangled issues by analyzing images and highlighting subtle parts that may otherwise be overlooked.
Using AI platforms that overlay on OCT imaging data, physicians receive immediate feedback during procedures. These systems can automatically identify plaque characteristics, assess vessel diameter, and even suggest optimal stent dimensions. The transformation is profound: what was once a nerve-racking and off-putting process—where doctors had to sort through overwhelming amounts of data manually—is now made significantly smoother by AI assistance.
Key elements of this technology include:
- Real-time analysis: AI algorithms rapidly process imaging data, ensuring that any critical conditions are flagged immediately.
- Actionable insights: The system recommends further steps, such as validating stent placement or adjusting the strategy in order to tackle any unexpected complications.
- Support for clinical expertise: Far from replacing the trained eye of specialists, AI augments expertise by providing additional layers of analysis.
Precision in Stenting with AI: Tackling the Tricky Parts of Vessel Analysis
One of the most exciting developments in recent years is the ability of AI to enhance precision in stenting procedures. Stenting, a common intervention for treating arterial blockages, has always been challenged by the need to match device specifications with the subtle differences in patient-specific anatomy. The fine points of accurately measuring vessel diameters and accounting for variations in plaque distribution were once a source of frustrating inconsistency.
AI-enabled systems address these tricky parts and tangled issues by automatically measuring the lumen and suggesting not only the correct stent length, but also the proper diameter. For instance, Abbott’s Ultreon 2.0 Software exemplifies such advancements by merging OCT imaging with AI algorithms to deliver targeted recommendations with an exceptional degree of precision.
Here, the benefits of AI-enhanced stenting are twofold:
- Reduction in post-procedure complications: By selecting stents that are closely aligned with the natural vessel dimensions, the risk of restenosis and other complications decreases.
- Improved long-term outcomes: Patients receive treatments that are tailor-made, reducing the likelihood of follow-up interventions and enhancing overall cardiovascular health.
Over time, such comprehensive integration of AI in vessel measurement and stent selection is expected to lead to consistently better clinical outcomes, as decision-making becomes more data-driven and less reliant on estimations made in the heat of the moment.
Enhanced Workflow Efficiency: Getting Through the Confusing Bits of Cardiac Interventions
Another key benefit of AI-enhanced cardiovascular imaging is the increase in workflow efficiency within the cath lab. In high-volume centers, where every minute counts, the ability to automate and standardize measurements offers enormous potential. Physicians can now get around the confusing bits of manually competitive assessments, leading to both speed and accuracy in planning and executing procedures.
Automated measurements provided by AI systems help in minimizing procedural variability. This means that regardless of the complexity involved, there is a consistent approach that every operator can follow. Eliminating the need for repeated manual interventions not only saves time but also helps in reducing the mental burden on physicians. In essence, AI is transforming the cath lab from a place of sometimes overwhelming decision-making into a more streamlined, data-driven environment.
For comprehensive clarity, consider the table below, which highlights the benefits of AI integration in the cath lab workflow:
| Aspect | Traditional Method | AI-Enhanced Approach |
|---|---|---|
| Speed | Time-consuming manual measurements | Rapid real-time analysis |
| Precision | Variability in interpretation | Consistent, objective data output |
| Workflow | Multiple steps requiring checks | Streamlined, automated procedures |
| Outcome Consistency | Tangled issues with uniformity | Standardized care protocols |
Preparing Your Facilities for AI Integration: Focusing on Staff Training and Infrastructure Readiness
The future of AI in cardiovascular care is promising, yet its successful implementation depends largely on how well healthcare facilities and professionals prepare for the transition. There are several operational areas that require attention in order to effectively harness the capabilities of AI-integrated imaging systems.
For hospitals looking to adopt these advanced technologies, it is essential to address the following focal points:
- Staff Training: Physicians and clinical staff need structured education that helps them understand where AI-generated insights intersect with traditional clinical data. Hands-on training in both live and simulated environments can build the necessary confidence.
- Infrastructure Readiness: Upgrading software platforms and ensuring interoperability between devices and electronic health records are essential for smooth integration. This includes upgrading network security and data-sharing capabilities so that AI tools can access and process vast amounts of real-time information.
- Interdisciplinary Collaboration: Bringing together experts from IT, biomedical engineering, and clinical leadership is key. This collaboration helps in addressing the confusing bits of deploying new technology and ensures that all stakeholders are on the same page regarding operational protocols.
Training and Simulation: Managing Your Way Through Training Challenges
Proper staff training is critical to the effective adoption of AI-enhanced imaging tools. In a field where every second counts and the stakes cannot be overstated, physicians must possess not only a deep understanding of traditional cardiovascular care but also be adept at using new technological aids. Training programs should include:
- Real-life scenarios: Doctors can benefit from simulations that allow them to apply AI insights in a controlled, low-risk environment.
- Ongoing education: Regular workshops and refresher courses help keep the team updated on the latest AI developments and data handling procedures.
- Cross-disciplinary training: Involving IT professionals in medical training sessions ensures a better comprehension of system functionalities and troubleshooting techniques.
This dynamic training approach helps medical staff find their way through the nerve-racking process of integrating cutting-edge technology into daily practice, ensuring scalability and sustainability in patient care.
Upgrading Infrastructure: Making Your Way Through the Isolated Details
The successful deployment of AI in cardiovascular imaging goes beyond just training—it also depends on building the right infrastructure. Healthcare systems must be ready to support heavy data loads, ensure seamless device integration, and provide strong cybersecurity measures. Some key steps include:
- Software Upgrades: Investing in modern software that supports AI algorithms is crucial for integrating with existing imaging equipment.
- Data Interoperability: Ensuring that all devices and software platforms communicate effectively reduces the chances of data silos, which can complicate decision-making.
- Network Security Enhancements: Protecting sensitive patient data and AI-generated information from breaches or cyberattacks is non-negotiable.
- Hardware Investment: Upgrading servers and high-performance computing systems enables real-time processing of large imaging datasets.
Addressing these smaller twists and turns is critical. The little details—from securing data-sharing capabilities to integrating cross-platform functionalities—can mean the difference between a successful AI rollout and a system riddled with tension. Hospitals that make these investments are laying the groundwork for a smoother transition into a digitally advanced future.
Challenges and Future Directions: Paving the Way for Predictive and Proactive Healthcare
While the integration of AI in cardiovascular imaging offers exceptional promise, it is also important to recognize that new technology inevitably comes with its own set of challenges. As with any innovative process, there are several tricky parts and intimidating hurdles that need to be addressed before broad-scale adoption becomes a reality.
One of the primary challenges in this space is ensuring that AI tools are integrated into clinical workflows without overwhelming healthcare professionals. For instance, while the benefits of automated plaque characterization and stent suggestion are clear, it remains essential that physicians still maintain ultimate decision-making authority. In other words, AI should support rather than replace the skilled judgment of trained professionals.
Another issue is the need for extensive validation and clinical trials. Before such new technology can be adopted universally, there must be comprehensive evidence demonstrating that AI-driven procedures lead to improved outcomes compared to traditional methods. This search for robust data requires a cooperative approach between clinicians, engineers, and regulatory bodies—a journey that might seem intimidating at first due to its nerve-racking complexities.
Future of Predictive Imaging: A Closer Look at Next-Generation Techniques
The evolution of AI in cardiovascular imaging is only at its beginning. Once physicians become comfortable using AI as a decision-support tool in the cath lab, the next step will be implementing predictive imaging techniques. This involves computing the resistance to blood flow in blocked arteries, which could help clinicians zero in on the most critical areas needing intervention.
Predictive imaging is set to radically change the landscape of cardiovascular health management by not only guiding procedures, but also by providing insights into long-term patient outcomes. For example, by forecasting potential risks before they arise, AI can facilitate pre-emptive measures to prevent complications. This proactive approach is key to reducing readmission rates and ensuring sustainable health improvements.
Emerging techniques in predictive imaging aim to:
- Forecast patient-specific risks: Utilizing historical patient data to project future cardiovascular events.
- Optimize treatment plans: Tailoring interventions based on predictive models to enhance patient safety and efficiency.
- Improve resource allocation: Helping hospitals prepare for high-risk cases and allocate resources appropriately.
Although the pathway towards predictive imaging might seem full of problems and loaded with issues, the potential benefits—faster interventions, reduced procedural errors, and personalized care—make it an essential area of research and development.
Bringing Beyond the Cath Lab: AI in Long-Term Patient Management
The transformative effects of AI are not limited to the cath lab. In fact, the same technologies that empower physicians during interventions have the potential to revolutionize long-term patient management. AI can assist in monitoring patients remotely, analyzing trends over time, and providing customized recommendations to maintain cardiovascular health.
Remote patient monitoring (RPM) solutions, powered by AI, enable continuous collection of patient data. These systems can flag subtle details in heart rate variability, blood pressure, and other key indicators that might otherwise slip through the cracks during routine check-ups. With this approach, healthcare providers can manage care more effectively by:
- Early detection of complications: AI algorithms can detect slight changes in patient data that may indicate an impending cardiovascular event.
- Customized care plans: Data-driven insights allow the creation of tailored treatment plans that address individual patient needs over time.
- Improved patient adherence: Continuous feedback and alert systems encourage patients to stay engaged with their treatment protocols.
Ultimately, the integration of AI into long-term management strategies represents a shift from reactive to proactive healthcare. Although the initial learning curve can be overwhelming for both patients and providers, the potential for improved outcomes and enhanced quality of life is super important in the evolution of personalized medicine.
Combining Human Expertise with Technological Advancements: The Road Ahead
While the promise of AI in the field of cardiovascular imaging is undeniable, it is equally vital to remember that technology is only as effective as the people who wield it. The future of healthcare depends on a delicate balance between cutting-edge digital solutions and the nuanced expertise of medical professionals. Achieving this balance calls for a dual commitment to rigorous training and ethical application of new tools.
Healthcare professionals are encouraged to embrace these advancements by actively participating in training sessions and workshops, while institutions must invest in robust technological infrastructure. As AI applications become more mainstream, the improvement of patient outcomes will require medical practitioners to continuously sort out the little details where technology intersects with human judgment.
Here are some practical steps for blending technology with clinical practice:
- Continued professional development: Regular courses and hands-on training ensure that clinicians get into the fast pace of digital innovation without losing the human touch essential to patient care.
- Ethical oversight: Establishing committees and protocols to review the application of AI tools can help ensure that innovations are applied responsibly and transparently.
- Patient engagement: Educating patients about the benefits, limitations, and safety measures of AI in their care can build trust and encourage collaborative decision-making.
By combining human intuition with technological efficiencies, the field of cardiovascular care can rise to meet the demands of an increasingly data-driven era. This balanced approach means that while AI helps traverse the nerve-racking twists and turns of complex procedures, the ultimate authority remains with the human expert well-versed in the art of medicine.
Conclusion: The Road Ahead for AI in Cardiovascular Medicine
As we stand on the threshold of what promises to be a revolutionary change in cardiovascular medicine, it is clear that AI is more than just a sophisticated tool—it represents a movement toward truly personalized, precise, and proactive care. AI-driven OCT imaging is paving the way for faster, safer, and more accurate interventions by easing the tricky parts of plaque characterization and ensuring precision in stenting procedures.
While there are still nerve-racking challenges along the way and one must figure a path through the overwhelming requirements of data infrastructure and staff training, the benefits of this integration are too significant to ignore. Healthcare institutions and medical device developers alike must take the wheel in adopting these innovations responsibly and ethically.
Looking into the future, we see a landscape where AI not only transforms the cath lab but also redefines the way we think about preventive care. With predictive imaging and continuous remote monitoring, AI is set to revolutionize long-term patient management—ensuring that timely, personalized interventions become the norm rather than the exception.
In summary, the journey toward fully integrated AI solutions in cardiovascular care is full of both remarkable potential and challenging twists and turns. As medical professionals, embracing these intelligent systems while maintaining a firm grasp on human expertise will be super important. The evolution of AI-enhanced imaging is not merely a tale of technological triumph, but a story of collaborative progress—one where digital innovation meets empathetic patient care.
By investing in advanced training, upgrading infrastructure, and fostering interdisciplinary collaborations, healthcare providers can successfully manage their way through the confusing bits and take full advantage of what AI has to offer. As we look to tomorrow, it is our collective responsibility to ensure that the benefits of these innovations are widely accessible, ethically implemented, and continually refined in the service of improved patient outcomes.
Adopting AI in cardiovascular imaging is not without its challenges, but its potential to transform patient care makes it an essential step forward. With robust support systems in place and a clear focus on maintaining the balance between technology and human expertise, the future of cardiovascular medicine looks brighter than ever.
The journey ahead may be intricate and full of nerve-racking decisions, yet every step forward brings us closer to delivering the kind of proactive, data-guided care that will define the next generation of cardiovascular intervention. As both technology and clinical practices advance hand in hand, the healthcare landscape will inevitably move toward a more efficient, accurate, and compassionate model of patient care.
Ultimately, the conversation about AI in cardiovascular imaging is not just about technology—it’s about reshaping the very fabric of medical care. From enhancing the precision of interventional procedures to supporting long-term management and predictive diagnostics, AI is at the heart of a broader movement toward smarter, faster, and more patient-focused healthcare. By welcoming these advancements with a balanced approach that respects both innovation and the indispensable value of clinical experience, we can look forward to a future where every patient receives care that is as personalized as it is precise.
Originally Post From https://www.mpo-mag.com/exclusives/the-advancing-role-of-ai-in-cardiovascular-imaging/
Read more about this topic at
Revolutionizing Medical Imaging: The Transformative Role of …
AI’s Transformative Power: A Revolution in Medical Imaging