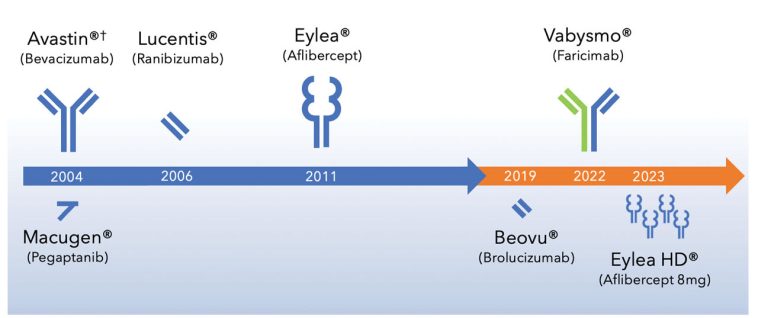
Faricimab in Neovascular Age-Related Macular Degeneration: A New Chapter in Therapy
In the ever-evolving world of ophthalmology, the emergence of faricimab as a secondary treatment for neovascular age-related macular degeneration (nAMD) has stirred considerable interest. This opinion editorial takes a closer look at how faricimab offers promising structural benefits, along with its potential to extend treatment intervals and maintain stable functional outcomes—as compared to the currently used anti-vascular endothelial growth factor (anti-VEGF) therapies.
While many practitioners have long relied upon traditional anti-VEGF agents, the tricky parts in managing persistent nAMD have prompted the exploration of alternative therapies. In a recent systematic review and meta-analysis, researchers observed that patients with nAMD treated with faricimab experienced significant reductions in central macular thickness (CMT) and pigment epithelium detachment (PED) height, without causing a dramatic change in visual acuity. The discussion here dives into the twisted issues, subtle details, and the fine points regarding the use of faricimab, offering insight into its future role.
Alternative Options to Traditional Anti-VEGF Therapy
One of the key takeaways from research on faricimab is its efficacy in patients who have grown tired of their current treatments. The option to switch to faricimab caters to those who are not getting optimal results with earlier anti-VEGF agents or who are experiencing what some researchers call a “treatment resistance.” This new approach is aimed at artfully addressing the confusing bits that come with long-term management of nAMD.
Comparing Structural and Functional Outcomes
When examining any therapeutic intervention, it is essential to differentiate between structural improvements and functional outcomes. With faricimab, studies have showcased a notable decrease in the CMT values as well as PED height:
- Central Macular Thickness: Significant reductions at the 3-month and 6-month marks suggest that faricimab can help ease the problematic swelling in the macula.
- Pigment Epithelium Detachment: A reduction in PED height has been clearly documented, hinting at a positive structural response by the retina.
- Visual Acuity: Interestingly, the best corrected visual acuity (BCVA) improvements were not statistically significant, illuminating the twist and turns encountered when linking anatomical improvements with functional recovery.
These findings underline the essential point that while faricimab’s effects on the retina’s structure can be measured quite definitively, the link to improved vision is more subtle—a reminder that medicine often involves a balance of beneficial outcomes and remaining challenges.
Evaluating the Evidence: A Comprehensive Meta-Analysis Perspective
The systematic review and meta-analysis that forms the backbone of these observations gathered data from over 20 studies involving more than 1000 eyes with nAMD. The studies were meticulously sorted out to provide a clear picture of how faricimab stacks up against traditional therapies. Such large-scale reviews are vital because they help both clinicians and researchers make their way through the tangle of available evidence, presenting a balanced view.
Key Findings and Statistics
To get a closer look at the statistics:
| Outcome | Time Point | Mean Difference (µm or Weeks) | 95% Confidence Interval | p-value |
|---|---|---|---|---|
| Central Macular Thickness (CMT) | 3 months | −47.08 µm | (−66.01, −28.15) | 0.009 |
| CMT | 6 months | −44.68 µm | (−67.17, −22.20) | 0.002 |
| Pigment Epithelium Detachment (PED) Height | 3 months | −31.71 µm | (−45.12, −18.30) | 0.036 |
| PED Height | 6 months | −34.85 µm | (−50.19, −19.51) | 0.011 |
| Extended Treatment Interval | Overall | +1.87 weeks | (0.41, 33.3) | 0.019 |
While these numbers are promising, they also highlight that significant structural improvements do not always translate directly into superior vision results. This subtle difference is an important discussion point for clinicians, given that the ultimate aim is to enhance both anatomical appearance and quality of vision.
Understanding the Subtle Differences: Structural Gains Versus Functional Vision
In any treatment for nAMD, it is important to consider both the little twists associated with anatomical changes and the slight differences in actual visual performance. With faricimab, we see that although the retina’s physical structure improves measurably, best corrected visual acuity remains largely unchanged. In plain language, the therapy seems to stabilize the hardware of the eye while offering only limited changes in the software—as in visual function.
This observation raises important questions: Is the stabilization of retinal structure a harbinger of longer-term benefits in vision? Or does it simply indicate that while the condition’s physical markers can be modified, the nerve-racking challenge of restoring full visual function remains unresolved? The answer may lie in longer follow-up studies and more extensive real-world data that focus on patient-reported outcomes and quality of life.
Pros and Cons of Implementing Faricimab in Clinical Practice
Given the promising yet somewhat mixed results, let’s break down the pros and cons of incorporating faricimab as a second-line therapy for nAMD.
Advantages of Faricimab Adoption
- Structural Benefits: The significant reduction in CMT and PED height is a strong indicator that faricimab can effectively manage the anatomical signs of nAMD.
- Extended Treatment Intervals: For many patients, fewer injections mean less discomfort and reduced clinic visits, which is both cost-effective and time-saving.
- Low Incidence of Serious Side Effects: Safety profiles from various studies suggest a relatively low rate of serious adverse events, making it a candidate for broader clinical use.
- Alternative for Recalcitrant Cases: Patients experiencing a less-than-optimal response to existing anti-VEGF agents may find faricimab a welcomed alternative.
Potential Drawbacks and Considerations
- Stable Functional Outcomes: The lack of significant improvement in visual acuity calls for caution, as structural improvements do not automatically mean better vision quality.
- Long-Term Efficacy: More data from long-term studies are needed to establish whether the apparent benefits can be sustained over time.
- Cost Implications: With any new treatment, the financial aspects—including insurance coverage and out-of-pocket expenses—need careful examination.
- Adaptation and Familiarity: The transition from well-known anti-VEGF therapies to a dual-action agent like faricimab may require further training and a period of adjustment for practitioners.
Exploring Personalized Treatment Strategies in nAMD
One of the most promising aspects of faricimab is its role in personalized medicine. As physicians get more comfortable with the dual-action approach provided by faricimab, there is potential to tailor treatments based on individual patient profiles. The extended treatment intervals, in particular, could be adapted to suit patients’ lifestyles and compliance levels.
Below is a table summarizing potential personalized strategies based on patient characteristics:
| Patient Profile | Potential Benefit | Considerations |
|---|---|---|
| Patients with Recalcitrant nAMD | Option to switch to faricimab for better structural outcomes | Monitor BCVA closely; regular follow-ups are crucial |
| Elderly Patients with Limited Mobility | Extended treatment intervals reduce the need for frequent injections | Ensure that logistical support for follow-up visits is in place |
| Patients Sensitive to Injection Frequency | Reduced appointment burden with extended intervals | Keep a close watch on the long-term stability of the retina |
| Patients with Prior Anti-VEGF Exposure | Switching may provide an alternative approach when traditional treatments plateau | Evaluate overall treatment response periodically |
Tailoring therapy in this manner not only addresses the nail-biting challenges of standard treatment protocols but also better accommodates the unique needs of each patient. Such patient-focused strategies can help clinicians figure a path through the tangle of available treatments in the management of nAMD.
Practical Considerations for Clinicians and Patients
As far as implementing faricimab in routine clinical practice, both clinicians and patients should be aware of several nerve-racking details. First, while the therapy demonstrates strong anatomical benefits, and extended treatment intervals can indeed be a game-changer in terms of convenience, there is a need for more research on the long-term visual outcomes.
For clinicians looking to adopt faricimab, here are some key points to consider:
- Patient Selection: Not every patient may be an ideal candidate. Those with known treatment resistance or those experiencing sub-optimal responses with traditional anti-VEGF therapies might see better structural improvements.
- Monitoring Protocols: Given the steady structural benefits without a parallel significant improvement in visual acuity, regular imaging studies and vision assessments remain critical to ensure that the administered therapy is producing the desired overall outcomes.
- Cost and Accessibility: The expense of newer therapies can be intimidating. Both practitioners and patients should ascertain cost-effectiveness and available reimbursement options.
- Adverse Events: Although the reported adverse events have been low, clinicians must maintain vigilance—particularly in a landscape where individual responses can vary.
For patients, it may be helpful to understand that transitioning to a new treatment option is as much about quality of life as it is about clinical efficacy. Reduced injection frequency, even if it comes with limited improvement in visual acuity, means fewer visits to the treatment center and potentially less anxiety about the procedure.
Future Directions: Research and Real-World Evidence
As with many next-generation therapeutics, the journey of faricimab is on an upward trajectory. The current body of real-world evidence is promising, yet it remains full of problems that call for further exploration. Researchers are now encouraged to:
- Conduct Long-Term Follow-Up Studies: More extended observation periods will help determine whether the structural benefits eventually translate into practical improvements in daily living and vision tasks.
- Investigate Combination Therapies: There is growing interest in exploring whether combining faricimab with other therapeutic approaches might overcome the limitations currently observed in functional outcomes.
- Examine Cost-Effectiveness: Detailed budget impact analyses are needed to gauge the real-world sustainability of faricimab treatment over many years, particularly in healthcare systems with constrained resources.
- Leverage Advanced Imaging: Modern imaging techniques could be integrated to provide better insights into the subtle details of retinal changes during treatment.
The research community continues to dig into the promising early results by working through the tricky parts of study design and statistical interpretation. Each new study helps piece together the larger picture of how best to manage nAMD, offering hope that eventually the gap between structural and functional outcomes will close.
Patient Case Scenarios: Real-World Experiences
To further ground this discussion, it is important to shed light on real-world experiences. For example, consider a middle-aged patient who was initially on traditional anti-VEGF therapy but experienced only modest improvements. Upon switching to faricimab, the patient noticed:
- An appreciable decrease in retinal swelling (as documented by imaging studies).
- A noticeable extension in the period between needed treatments, which in turn reduced clinic visits.
- Stable overall vision, albeit without dramatic improvement in clarity.
While such cases are promising, they also underscore that faricimab does not provide a magic bullet. Instead, it represents an important, alternative tool—a must-have option—for managing patients who might be stuck in the confusing bits of conventional treatment.
Expert Opinions and Clinical Insights
Leading retina specialists have expressed cautious optimism about the role of faricimab. Many experts view the therapy as a meaningful stepping stone in overcoming the subtle challenges that have long hampered the treatment of nAMD. One common perspective among these clinicians is that faricimab’s dual mechanism, which targets both VEGF-A and angiopoietin-2, provides a broader approach to managing the tangled issues inherent in nAMD.
Experts also note that while the improvement in anatomical markers is evident, the small distinctions in visual outcomes warrant further investigation. Future trials may help to unearth whether more aggressive or earlier adoption of faricimab can lead to greater functional gains. For now, the therapy appears to offer a balanced solution—one that reduces the strain of frequent visits and has the potential to be further refined as more long-term data become available.
Broader Implications for Ophthalmic Practice
The incorporation of faricimab into treatment protocols carries broader implications for ophthalmic practice. Its introduction may inspire clinicians to reexamine existing treatment pathways and consider more personalized management strategies for nAMD. For instance, the significant reduction in structural markers might prompt a shift in focus from solely improving vision to also preserving the underlying tissue health of the retina.
This could lead to a paradigm where treatments are no longer seen as a choice between a rapid fix or long-term stability, but instead as a balanced strategy where both aspects are carefully weighed. As the medical community takes a closer look at these promising developments, it becomes increasingly clear that faricimab has the potential to reshape the treatment landscape for nAMD.
Concluding Thoughts: Steering Through the Future of nAMD Treatment
In summary, faricimab presents an exciting new frontier in the treatment of neovascular age-related macular degeneration. It offers scared-of-the-unknown benefits in terms of significant structural improvements and the convenience of extended treatment intervals. However, it also brings with it a series of challenging questions regarding the translation of these anatomical gains into measurable improvements in visual function.
The fine points of this discourse remind us that modern medicine, much like navigating a maze of tangled issues, is rife with both breakthroughs and challenges. As clinicians and researchers continue to dig into patient data and refine treatment strategies, the hope remains that faricimab may serve as an essential adjunct in managing one of the most complex ocular conditions of our time.
By embracing new therapies while remaining mindful of the nerve-racking uncertainties inherent in innovative treatments, the ophthalmology community can continue to improve outcomes for patients with nAMD. The journey forward will likely require more long-term data, ongoing dialogue among experts, and above all, a willingness to work through the subtle details that define the landscape of modern eye care.
Ultimately, faricimab is more than just another drug in the pharmaceutical arsenal. It is a beacon of hope for many patients who have struggled with the overwhelming nature of conventional treatment strategies. Its dual-action mechanism, coupled with the convenience of fewer injections, could well pave the way for a future where managing complicated retinal conditions is less nerve-racking and more sustainable. Only time will tell if these anatomical advantages translate into a full spectrum of meaningful, everyday benefits for patients.
For now, clinicians are advised to take a measured approach—evaluating each patient’s unique profile, weighing the pros and cons, and making informed choices based on comprehensive meta-analytical data and real-world outcomes. In doing so, the ophthalmology community can continue to advance and refine treatment protocols that address both the visible and hidden complexities of nAMD.
Originally Post From https://www.nature.com/articles/s41433-025-03943-7
Read more about this topic at
Short-term outcomes of treatment switch to faricimab in …
Real-world six-month outcomes in patients switched to …