Clinical Clustering in Pediatric Behçet Disease: A New Approach to Personalized Treatment
Modern medicine continues to face tricky parts in diagnosing and treating rare, multisystem conditions. Pediatric Behçet disease, with its tangled issues and subtle parts, has long baffled clinicians with its unpredictable symptom profile and regional variations. Recent research using cluster analysis has opened up promising avenues to tailor treatments for young patients. In this editorial, we take a closer look at how clinical clustering may revolutionize the approach to this complex condition.
The study in focus evaluated 600 pediatric patients (diagnosed before 18 years of age), drawing data from Turkey, Iran, and several European centers. The analysis unearthed seven distinct clinical clusters based on symptom involvement. This exploration not only illuminates the fine points of how Behçet disease manifests in children, but also ignites a discussion on personalized treatment strategies that are key to improving outcomes.
Understanding Pediatric Behçet Disease: The Background
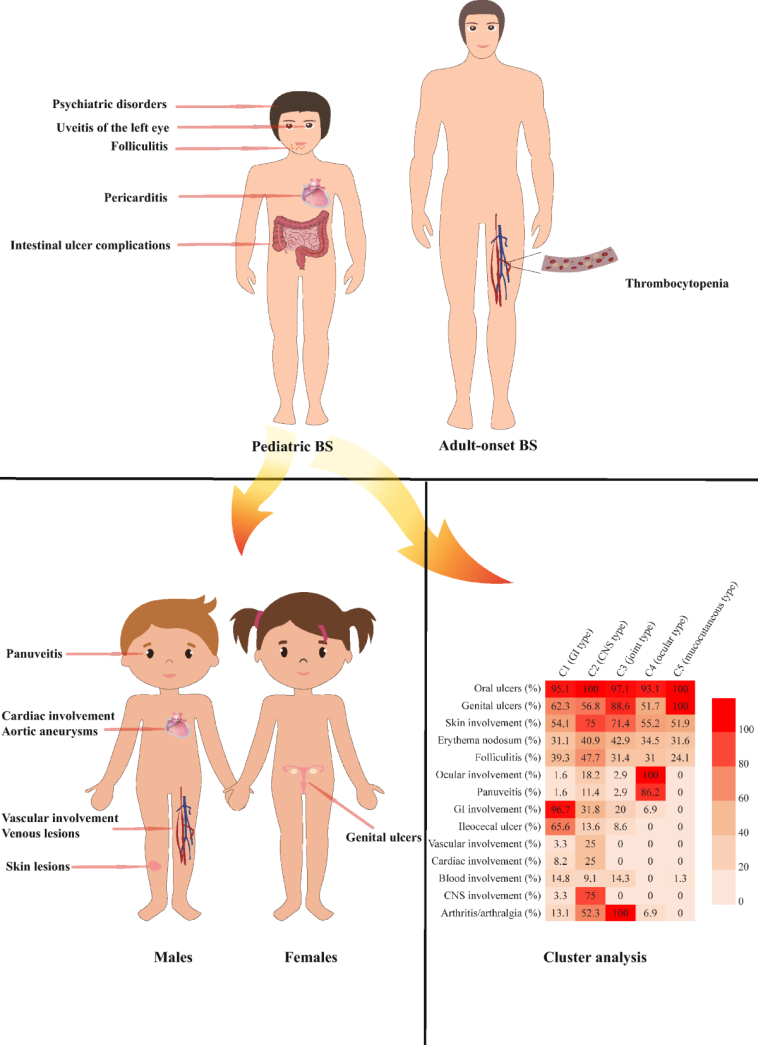
Behçet disease is a rare inflammatory vasculitis that has long been misunderstood due to its intimidating and complicated pieces. Primarily affecting the mucocutaneous regions—skin and mucous membranes—it also features manifestations in ocular, musculoskeletal, neurologic, vascular, gastrointestinal, and even cardiac systems. The highly variable presentations of the disease have made it difficult for physicians to predict outcomes and decide on the best treatment options.
Among children, the stakes are even higher. Diagnosing a condition that presents with a mix of confusing bits across multiple systems can be nerve-racking for both caregivers and clinicians. The median age for diagnosis in the study was 14.4 years, with a near-equal distribution between boys and girls. Such data underline the importance of early detection and tailored management strategies—which are now being refined thanks to a closer look at clinical clusters.
Decoding the Clusters: What the Study Revealed
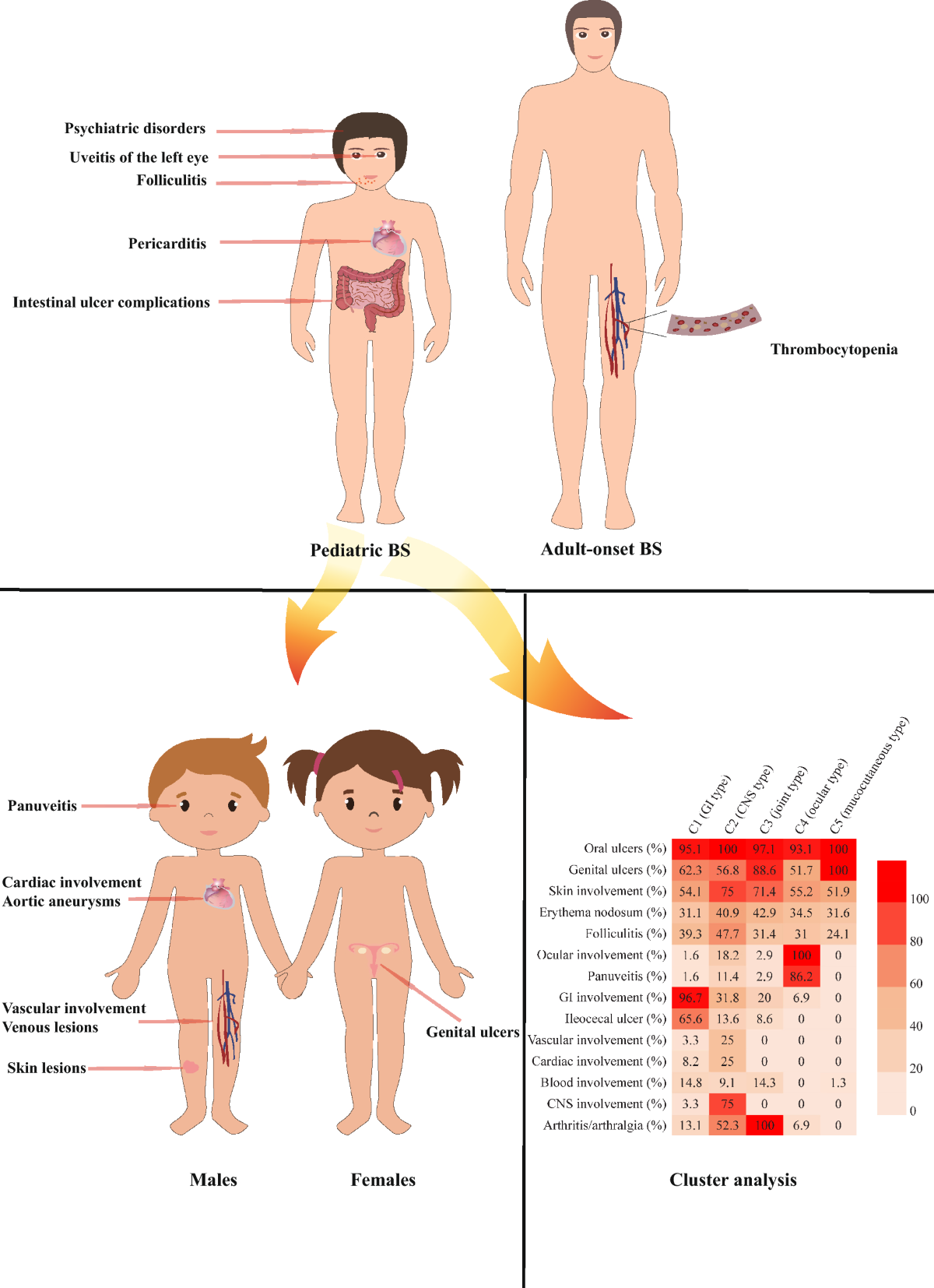
The research deployed hierarchical and k-modes cluster analyses to group patients based on their clinical presentations. The seven distinct clusters identified are:
- Vascular Cluster: Young patients with predominant vascular involvement.
- Mucocutaneous-only Cluster: Cases where skin and mucosal manifestations dominate.
- Ocular Cluster: Patients with significant eye involvement.
- Gastrointestinal Cluster: Those presenting with gastrointestinal symptoms.
- Mixed Cluster: A combination of various system involvements.
- Neurologic-Ocular Cluster: Cases presenting with symptoms in both neurological and ocular domains.
- Mucocutaneous-Musculoskeletal Cluster: Patients exhibiting both skin/mucosal and musculoskeletal issues.
Even though these clusters were defined by the predominant system involved, overlapping features were very common. Mucocutaneous symptoms, for example, were nearly universal, present in 87.5% to 100% of patients across all clusters. Recognizing these shared aspects helps clinicians figure a path through the tangled issues inherent in the disease and paves the way for a more flexible and tailored treatment approach.
Geographic Influences: How Location Shapes the Disease Profile
One of the study’s key insights is that geographic region plays a super important role in determining the clinical features of pediatric Behçet disease. The regional differences observed demonstrate that patients from different areas often display varying symptom profiles:
- Iran: A heightened prevalence of ocular involvement was recorded, with 63.7% of Iranian patients experiencing eye-related complications.
- Turkey: Musculoskeletal and vascular manifestations were more common, noted in 56.3% and 19.9% of patients respectively.
- Europe: Gastrointestinal symptoms led the way, with a notable 25.4% of European patients reporting digestive issues.
This data suggests that certain geographic factors, such as genetic predispositions or environmental triggers, may contribute to the subtle differences in how pediatric Behçet disease manifests. These findings encourage clinicians to take a closer look at each patient’s background when formulating a treatment plan, as the fine shades in clinical presentation are often influenced by regional factors.
Personalized Therapy: Tailoring Treatment to Clinical Clusters
With an increasing emphasis on personalized medicine, understanding these clinical clusters is key to designing treatment regimens that address the nerve-racking twists and turns of pediatric Behçet disease. Different clusters not only present with distinct symptoms but also show varied responses to treatments.
For instance:
- Colchicine: This was the most commonly prescribed therapy, reaching about 73.2% of the patient cohort. Its widespread use across multiple clusters underscores its role as a must-have in managing mucocutaneous symptoms.
- Systemic Corticosteroids and Immunosuppressants: These were more frequently administered in clusters where ocular, vascular, or neurological features were predominant. Agents like azathioprine and methotrexate appeared as the preferred choices for controlling inflammation in more severe presentations.
- Biologic Therapies: Utilized mostly in the neurologic-ocular cluster, these advanced therapies offer hope where conventional treatments may fall short. Though their use was noted across all clusters, the nuanced differences in response underscore the need for a tailored approach based on the specific cluster identification.
By carefully dissecting the little details of how symptoms cluster together, medical professionals can recommend specific treatments that not only address the visible issues but also offer an improved overall prognosis. The study found that almost half the patients (47.8%) achieved remission during treatment, while a smaller percentage (11.4%) managed remission off therapy – reinforcing the importance of dynamic treatment plans in addressing both immediate and long-term patient well-being.
Recognizing the Hidden Complexities: What This Means for Clinicians
Pediatric Behçet disease is no stranger to confusing bits when it comes to its presentation. The study clearly demonstrates that the disease is piled with subtle parts that require a nuanced understanding. For clinicians, this means:
- Comprehensive Assessment: Physicians need to dig into each patient’s full profile, beyond mere surface symptoms, to capture the nitty-gritty details of their condition.
- Long-term Follow-Up: With a median follow-up period of three years, maintaining consistent monitoring is essential to adjust treatment strategies as the disease evolves.
- Family History and Genetic Markers: A family history of Behçet disease was found in 17.6% of patients, and over half were positive for the HLA-B51 marker. Such factors are key to figuring a path for personalized diagnosis and management.
Essentially, by breaking down the complicated pieces of the patient’s clinical picture and accurately categorizing them into clusters, clinicians can develop a step-by-step guide to treatment that is both individualized and flexible. This kind of methodological approach enhances the potential for achieving remission and managing relapses effectively.
Comparing Treatment Strategies: Evidence-Based Trends
A closer look at the treatment patterns across different clusters reveals a landscape that is both diverse and interconnected. To help organize this complex information, the table below summarizes the therapies used and the clusters in which they are most prevalent:
| Clinical Cluster | Predominant Therapy | Notable Features |
|---|---|---|
| Vascular | Corticosteroids, Immunosuppressants | Risk of vascular complications, requires timely intervention |
| Mucocutaneous-only | Colchicine | Consistent mucocutaneous symptoms with high remission rates |
| Ocular | Azathioprine, Methotrexate | High prevalence in Iran; demands careful monitoring to prevent vision loss |
| Gastrointestinal | Tailored Immunosuppressive Regimens | Highest rates in Europe; digestive management is crucial |
| Mixed | Combination Therapies | Multiple system involvement, requiring a multidrug approach |
| Neurologic-Ocular | Biologic Therapies along with Standard Immunosuppressants | Complex involvement of both neurological and ocular systems |
| Mucocutaneous-Musculoskeletal | Colchicine, with possible addition of Corticosteroids | Blend of skin and joint symptoms, often with promising treatment responses |
This table is a handy reference that underscores how treatment decisions are closely linked to the clinical cluster, thereby reducing ambiguous bits and providing clearer guidance on managing the patient’s condition.
Impact on Patient Outcomes: Achieving Remission
The study’s outcomes provide a promising picture when it comes to remission rates. Overall, close to half the patients achieved remission during treatment, and a smaller yet important group maintained remission even off therapy. While 8.4% experienced relapsing or refractory disease, the rates of such cases were lowest in the mucocutaneous-only and the mucocutaneous-musculoskeletal clusters.
These improvements in patient outcomes highlight that when clinicians take the time to sort out the different clusters and tailor treatments accordingly, there is a tangible positive impact. The tailored approach helps in:
- Reducing unnecessary medication exposure by targeting only the most needed therapies.
- Preventing long-term complications associated with poorly managed systemic inflammation.
- Enhancing the quality of life for young patients who might otherwise face a lifetime of intensive treatment protocols.
In an area full of problems and tense decision-making, these results offer a ray of hope to both healthcare providers and families dealing with this challenging condition.
Integrating Alternative Perspectives: The Role of Complementary Medicine and Nutrition
While the focus often remains on mainstream immunosuppressive and anti-inflammatory therapies, it’s also worth considering the role of alternative medicine and nutritional strategies in managing pediatric Behçet disease. Given the complexity and nerve-racking turns in the disease’s progression, integrating complementary strategies can sometimes help ease the overall burden of the illness.
Some of the key aspects that may be considered include:
- Diet and Nutrition: Anti-inflammatory diets rich in omega-3 fatty acids, antioxidants, and plant-based nutrients could potentially support overall immune function. Though data specific to Behçet disease remains limited, many clinicians advocate for nutritional counseling as part of a holistic treatment plan.
- Mind-Body Techniques: Practices such as guided meditation, yoga, or even acupuncture might help patients cope with the overwhelming stress of a chronic illness. These techniques can offer relief from the physical pain and the mental strain often associated with persistent inflammatory conditions.
- Complementary Therapies: Some studies suggest that certain herbal supplements might have modest antioxidant or anti-inflammatory effects. However, it is critical to evaluate these options on a case-by-case basis, ensuring they do not interfere with the primary therapeutic regimen.
Integrating these approaches should always be done under the supervision of healthcare professionals. They are not replacements for the must-have conventional treatments but can serve as valuable adjuncts in a comprehensive treatment strategy that aims to address both the visible symptoms and other subtle, underlying factors.
Practical Takeaways for Clinicians and Caregivers
For those working directly with pediatric patients experiencing Behçet disease, several practical strategies can help figure a path through the challenging landscape:
- Stay Informed on Regional Trends: Given the geographic differences in clinical presentation, it is critical to stay updated on local epidemiological data that might influence presentation and treatment strategies.
- Embrace a Multidisciplinary Approach: Collaborating closely with ophthalmologists, dermatologists, rheumatologists, and even alternative therapy specialists can enrich the overall care strategy.
- Personalize Treatment Plans: Rely on cluster-based classification to tailor therapy. Consider adjustments in immunosuppressive regimens based on each patient’s unique symptom composition.
- Educate Families: Since pediatric patients rely on caregivers, providing clear, relatable information on the disease’s twists and turns can reduce anxiety and help manage expectations.
By aligning treatment choices with the clusters identified in the study, healthcare providers can ultimately reduce the nerve-racking uncertainty that often accompanies managing such a multifaceted condition.
Addressing the Challenges: A Closer Look at Remaining Issues
Despite the promising insights, several challenging bits remain in the quest to fully harness the potential of clinical clustering in pediatric Behçet disease:
- Retrospective Study Limitations: The study’s design means that regional variability in clinical assessments might have influenced some of the findings. Moving forward, prospective research is essential to validate and refine these clusters.
- Overlap in Cluster Characteristics: Though the clusters provide a useful framework, overlapping features—like the near-universal presence of mucocutaneous symptoms—make it hard to draw absolute distinctions. Clinicians must continue to keep an open mind and adjust strategies based on evolving evidence.
- Tailoring Biologic Therapies: The optimal use of biologics in clusters such as the neurologic-ocular remains an area ripe for further investigation. Understanding the long-term outcomes of these targeted therapies requires careful, ongoing observation.
It is clear that the clinical landscape of pediatric Behçet disease is loaded with issues and that both research and practice must continually adapt. The adoption of a cluster-based approach represents a significant step forward, but it is only part of a broader ongoing effort to refine our understanding of the disease’s tricky parts.
Future Directions: Research and Policy Implications
Looking forward, several areas of research and policy must be addressed to improve outcomes in pediatric Behçet disease:
- Prospective Multicenter Studies: Future studies should aim for a prospective design to better capture the dynamic evolution of the disease over time. This approach will help reduce the confusing bits that arise from retrospective data collection.
- Enhanced Diagnostic Criteria: By incorporating these clinical clusters into diagnostic algorithms, healthcare providers can make more informed decisions—potentially reducing the overwhelming complexity often associated with diagnosing pediatric Behçet disease.
- Health Policy and Funding: Greater investment in research and access to advanced treatments is essential. Policymakers need to recognize the super important nature of pediatric autoimmune diseases and foster an environment where clinical innovation can thrive.
- Patient Registry Initiatives: Developing international registries with standardized data collection procedures can help navigate the myriad of subtle details and geographic influences. This will ultimately empower clinicians with richer data to guide patient care.
The advancements in cluster-based classification represent not only a promising clinical development but also call for shifts in how research, funding, and policy converge to support vulnerable pediatric populations. By prioritizing this area, the ultimate goal is to ensure that every child with Behçet disease receives a treatment plan as unique as their clinical presentation.
Conclusion: Charting a Path Through the Twists and Turns
Clinical clustering in pediatric Behçet disease has emerged as a promising roadmap to managing one of modern medicine’s most puzzling conditions. The study highlighted in our discussion underscores the importance of dissecting the tangled issues inherent in this disease and categorizing them into comprehensible, actionable clusters. With distinct groups such as vascular, mucocutaneous-only, ocular, gastrointestinal, mixed, neurologic-ocular, and mucocutaneous-musculoskeletal, clinicians now have an essential guide to formulating more personalized treatment plans.
While challenges remain—particularly regarding overlapping features and limitations of retrospective data—the move toward a more tailored approach offers renewed hope. From applying the best available evidence to integrating complementary therapies and addressing fine shades in patient histories, every step taken toward personalized care makes a difference in improving outcomes and quality of life.
For clinicians, caregivers, and policy-makers alike, the research invites us to work through the delicate balance between standardized treatment and customized care. In doing so, we are not just treating a disease; we are striving to create a future where every young patient can confidently step past the intimidating, often off-putting twists and turns of pediatric Behçet disease.
In our ever-evolving healthcare landscape, adopting a cluster-based approach to pediatric Behçet disease is a significant leap forward. As we continue to dig into the fine points and little details that separate one patient’s journey from another’s, the ultimate goal remains clear: to make well-informed, individualized care accessible to all, ensuring that every child receives the super important support they deserve.
Final Thoughts
The integration of clinical clustering into routine practice provides a refreshing and pragmatic perspective on an already difficult-to-manage disease. It equips clinicians with the tools needed to figure a path through the myriad of challenging symptoms, ensuring that treatment decisions are both evidence-based and patient-centered.
By embracing this nuanced approach—one that acknowledges the hidden complexities, respects regional differences, and promotes tailored therapies—we are stepping into an era of personalized medicine that should inspire healthcare providers to continuously pursue better outcomes for pediatric patients suffering from Behçet disease.
As with any emerging paradigm, continuous research, collaboration, and flexibility in treatment protocols are critical. In the end, working through the tricky parts of pediatric Behçet disease together may open new doors to relief and recovery, marking a turning point in our ability to manage and ultimately conquer this daunting condition.
Originally Post From https://www.rheumatologyadvisor.com/news/cluster-classification-in-pediatric-bd-may-help-personalize-treatment/
Read more about this topic at
Cluster headache – Diagnosis and treatment
Treatment of Cluster Headache: The American …